New Challenge for Doctors: Battling a Rare, Persistent Fungal Infection in the U.S.
Doctors are facing a new challenge: diagnosing and treating a highly persistent fungal infection that’s proving difficult to manage. In June 2024, the California Department of Public Health (CDPH) has reported the first known U.S. case of Trichophyton mentagrophytes genotype VII (TMVII), a rare dermatophyte infection. Like other dermatophytes, TMVII is a fungus that causes ringworm or tinea, leading to highly inflammatory, painful, and persistent lesions. This case, involving a patient who had traveled to California, marks a significant development in public health. These lesions often affect the genital, anal and oral areas and require prolonged treatment with oral antifungals. The infection poses a significant challenge due to its severity and persistence.


Wyatt Hanft, MD, MPH, an STI fellow at UCSF California Prevention Training Center, is leading CAPTC’s response efforts surrounding this challenge. Dr. Hanft has been instrumental in responding to TMVII and other related infections. He reflects, “In my role with CAPTC at UCSF, I have been responsible for creating educational materials for providers, some of which have involved TMVII. I’ve also been involved in discussions at both state and national levels regarding the TMVII case that was documented.”
The American Academy of Dermatology (AAD) has identified TMVII as a significant dermatophyte of concern, noting its transmission through sexual contact, particularly among men who have sex with men and those involved in sex tourism in Southeast Asia. TMVII can affect the genital area, buttocks, extremities, trunk, and face, and requires specialized testing like ITS genome sequencing for diagnosis. Treatment may involve oral terbinafine, but longer courses might be necessary, and in rare cases, oral itraconazole may be needed. The AAD advises healthcare providers to monitor patients closely, counsel them on transmission risks, and emphasize the need for adherence to prolonged therapy.
The first U.S. case of TMVII, diagnosed in New York in early 2024, involved a patient who became symptomatic in late 2023. Dr. Hanft explains, “[TMVII] was diagnosed in New York in early 2024 although the paper was published in June. It was a patient who initially became symptomatic in late 2023; they had a biopsy taken of the infection site, which identified a dermatophyte infection.” The complexity of diagnosing TMVII accentuates the necessity for advanced diagnostic techniques, as standard methods often fall short. “Unfortunately, with these types of infections…you can’t really tell the difference [with culture], so you need to sequence them to identify the genomic differences,” Dr. Hanft notes.
A critical aspect of addressing TMVII is reducing the stigma often associated with STIs. Dr. Hanft emphasizes that healthcare providers play a crucial role in normalizing discussions around sexual health and behaviors. “Healthcare providers should try to remove stigma from all STI-related health services that they provide. I think normalizing sexual behavior and what risks somebody might be at is helpful because the vast majority of the U.S. population is sexually active, and it’s something that needs to be talked about,” he asserts. By fostering an environment of openness and cultural competence, healthcare providers can ensure that patients feel comfortable seeking care and receiving appropriate guidance without fear of judgment.
The potential risk of local transmission in the U.S. is a significant concern. While TMVII is currently rare in the U.S., Dr. Hanft highlights the importance of vigilance. “It’s hard to say how significant the risk is currently, and what we do know is that TMVII is very rare in the U.S.; there’s only been one documented case,” he says. In Europe, the infection has shown the potential for local spread, with cases reported in countries like Germany, Austria, and France. Dr. Hanft advises, “Providers should be aware that this is an infection that could possibly affect people who are sexually active, and they should provide the appropriate work-up, treatment, and counseling if it’s indicated.”
The emergence of TMVII in the United States presents a new public health challenge, requiring coordinated efforts in clinical recognition, diagnosis, and treatment. Ongoing surveillance and research are essential to understanding the transmission dynamics and developing effective prevention strategies. Dr. Hanft emphasizes the need for improved public health surveillance and research, stating, “Trying to figure out how widespread [TMVII] is will be important. It would be helpful to understand what questions providers have regarding TMVII and what they are actually seeing in clinics.”
The emergence of Trichophyton mentagrophytes genotype VII in the United States reiterates the need for heightened awareness and early intervention in managing rare infections. As healthcare providers like Dr. Wyatt Hanft lead efforts to educate and equip their peers, reducing stigma around STIs becomes paramount to ensuring patients feel empowered to seek care. Through collaboration and innovation in public health strategies, the medical community can address this challenge while fostering an inclusive environment that prioritizes both prevention and treatment.




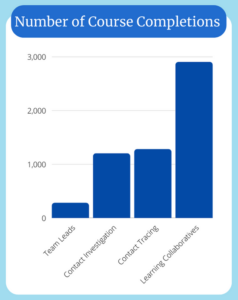 As a member of the National Network of Disease Intervention Training Centers (NNDITC), CAPTC developed curricula and delivered case investigation, contact tracing, and team leadership courses nationwide. CAPTC also introduced 13 Learning Collaboratives that complimented the NNDITC’s foundational Covid courses and directly addressed issues that case investigators (CI) and contact tracers (CT) encountered when interfacing with the public.
As a member of the National Network of Disease Intervention Training Centers (NNDITC), CAPTC developed curricula and delivered case investigation, contact tracing, and team leadership courses nationwide. CAPTC also introduced 13 Learning Collaboratives that complimented the NNDITC’s foundational Covid courses and directly addressed issues that case investigators (CI) and contact tracers (CT) encountered when interfacing with the public. “The ability to quickly distill the information and develop course material that was digestible to a widening range of people, was highly dependent on our ability to listen to the concerns expressed to the contact tracers and case investigators, and by them as well,” says Tafoya.
“The ability to quickly distill the information and develop course material that was digestible to a widening range of people, was highly dependent on our ability to listen to the concerns expressed to the contact tracers and case investigators, and by them as well,” says Tafoya.